Spatial Epidemiology of Infant Mortality: Mapping and Analyzing Geographical Variations and Determinants in Ethiopia Using EDHS Data
Conference
65th ISI World Statistics Congress
Format: CPS Abstract - WSC 2025
Keywords: "spatial, generalized linear models, geospatial
Session: CPS 29 - Spatial Determinants and Epidemiological Analysis in Children’s Health
Tuesday 7 October 5:10 p.m. - 6:10 p.m. (Europe/Amsterdam)
Abstract
Background: Infant mortality remains a significant public health challenge in Ethiopia. Examining infant mortality patterns can help track progress toward achieving the Sustainable Development Goals.
Objective: The study aimed to explore the geographical variations and associated factors of infant mortality in Ethiopia.
Method A total of 11,023 infants from the 2016 Ethiopian Demographic and Health Survey (EDHS) data were extracted and included in the analysis. The EDHS employed a two-stage cluster sampling design, with census enumeration areas as the primary sampling units and households as the secondary sampling units.
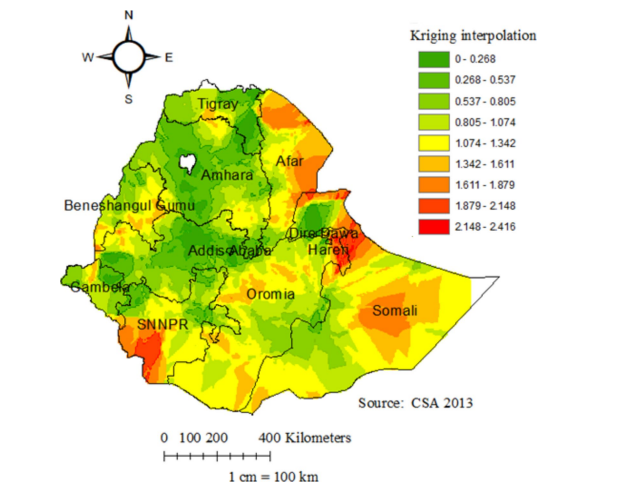
ArcGIS software was used for spatial analysis of the clusters to explore the geographical variations in infant mortality. A binary logistic regression analysis, conducted using R software, was employed to identify the significant determinants of infant mortality.
Results The spatial distribution of infant mortality was non-random across Ethiopia. Significant determinants of infant mortality included: not receiving antenatal care (AOR=1.45; 95%CI: 1.17, 1.79), not breastfeeding (AOR=3.94; 95%CI: 3.19, 4.81), poor household wealth (AOR=1.36; 95%CI: 1.04, 1.77), being a male infant (AOR=1.59; 95%CI: 1.29, 1.95), birth order of six or above (AOR=3.11; 95%CI: 2.08, 4.62), small birth size (AOR=1.27; 95%CI: 1.26, 1.60), short birth spacing (≤24 months, AOR=2.29; 95%CI: 1.79, 2.92 and 25-36 months, AOR=1.16; 95%CI: 1.12, 1.49), multiple births (AOR=6.82; 95%CI: 4.76, 10.81), rural residence (AOR=1.63; 95%CI: 1.05, 2.77), and living in the Afar (AOR=1.54; 95%CI: 1.01, 2.36), Harari (AOR=1.56; 95%CI: 1.04, 2.56), and Somali (AOR=1.52; 95%CI: 1.03, 2.39) regions.
Conclusions The study revealed a significant geographical disparity in infant mortality rates across the regions of Ethiopia, with the Afar, Harari, and Somali regions identified as hotspot areas with higher infant mortality. The key determinants of infant mortality in Ethiopia were lack of antenatal care (ANC) usage, not being breastfed, household poverty (poor wealth index), male sex of the infant, high birth order (6 or above), small birth size, short birth spacing, multiple births, rural residence, and living in the Afar, Harari, and Somali regions. These findings suggest that targeted interventions are needed in the identified hotspot regions to address the risk factors and alleviate the high infant mortality rates in these areas.
Figures/Tables
fig1
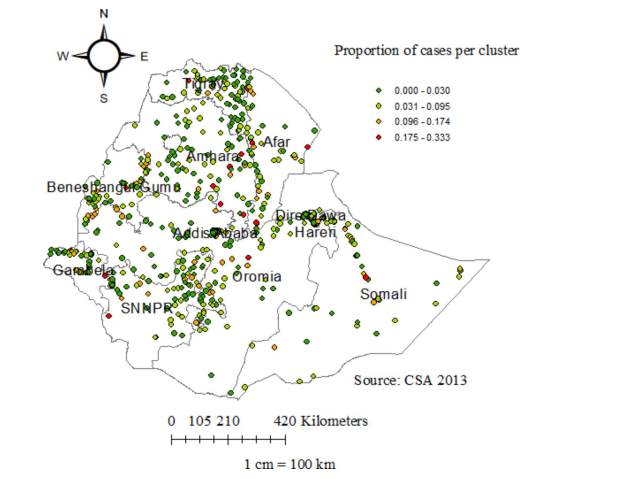
fig2